LIFESCAPES Medical BCI - Neurorehabilitation Device for Hand Paralysis after Stroke or Spinal Cord Injury

LIFESCAPES Medical BCI
A New Type of Rehabilitation Device that Measures Biosignals from the Head to Maintain, Develop, or Restore Muscle Strength in Fingers and Other Areas
LIFESCAPES Medical BCI is a new type of neurorehabilitation medical device designed for patients with various degrees of hand paralysis. It sensitively detects biosignals from the scalp and activates the robotic orthosis when appropriate motor intention is detected. To help patients perceive that the movement was generated by their own intention, electrical stimulation is applied to the agonist muscle. Each time the patient imagines the correct movement, precise feedback is provided through electrical stimulation and robotic assistance. Repetitive training aims to facilitate effective functional improvement.

Principles of BCI Rehabilitation
Principles of BCI Rehabilitation
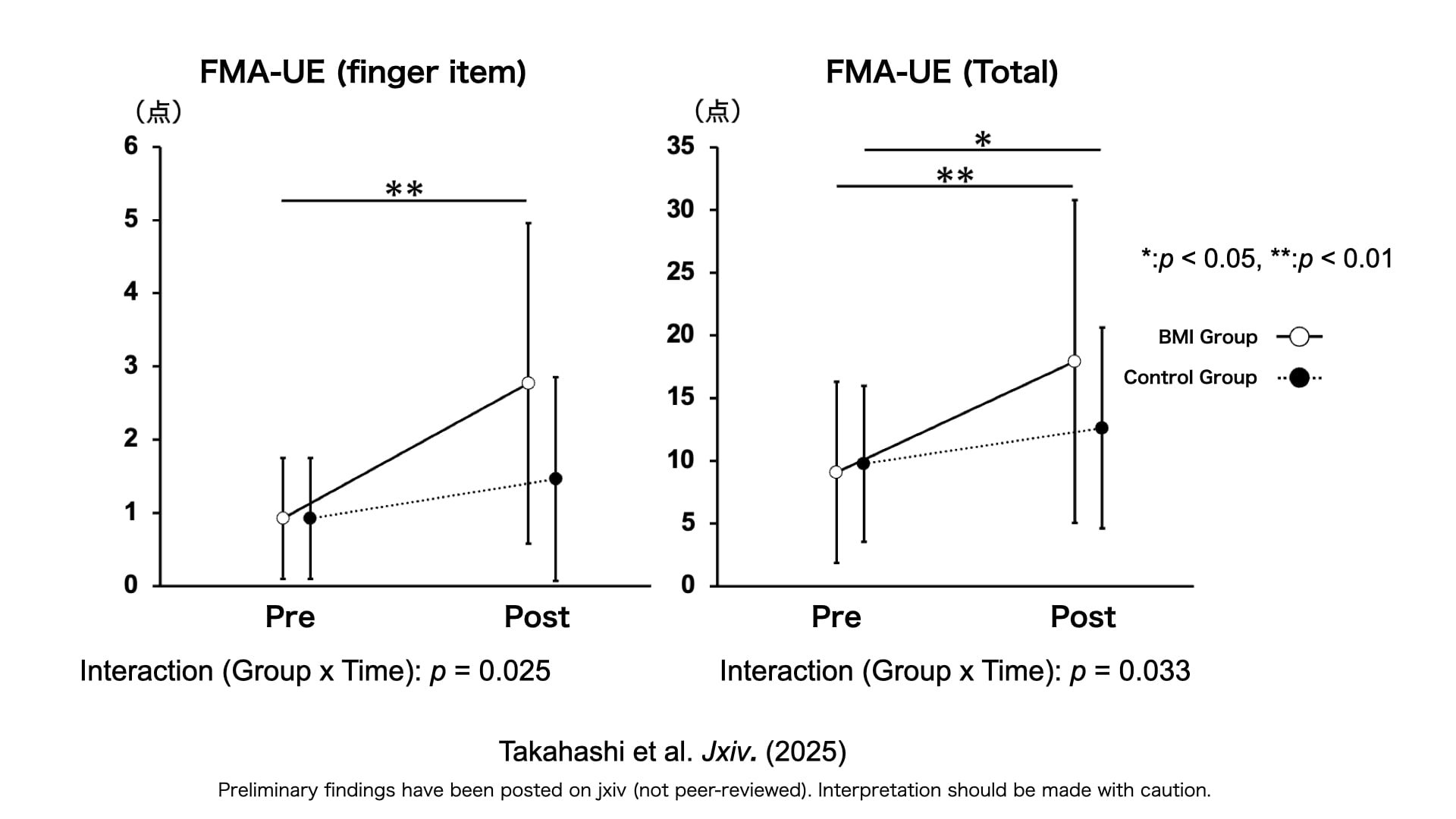
Changes in finger and upper limb motor function
Motor Function Recovery through BCI training | Muscle response in the target muscles is restored.
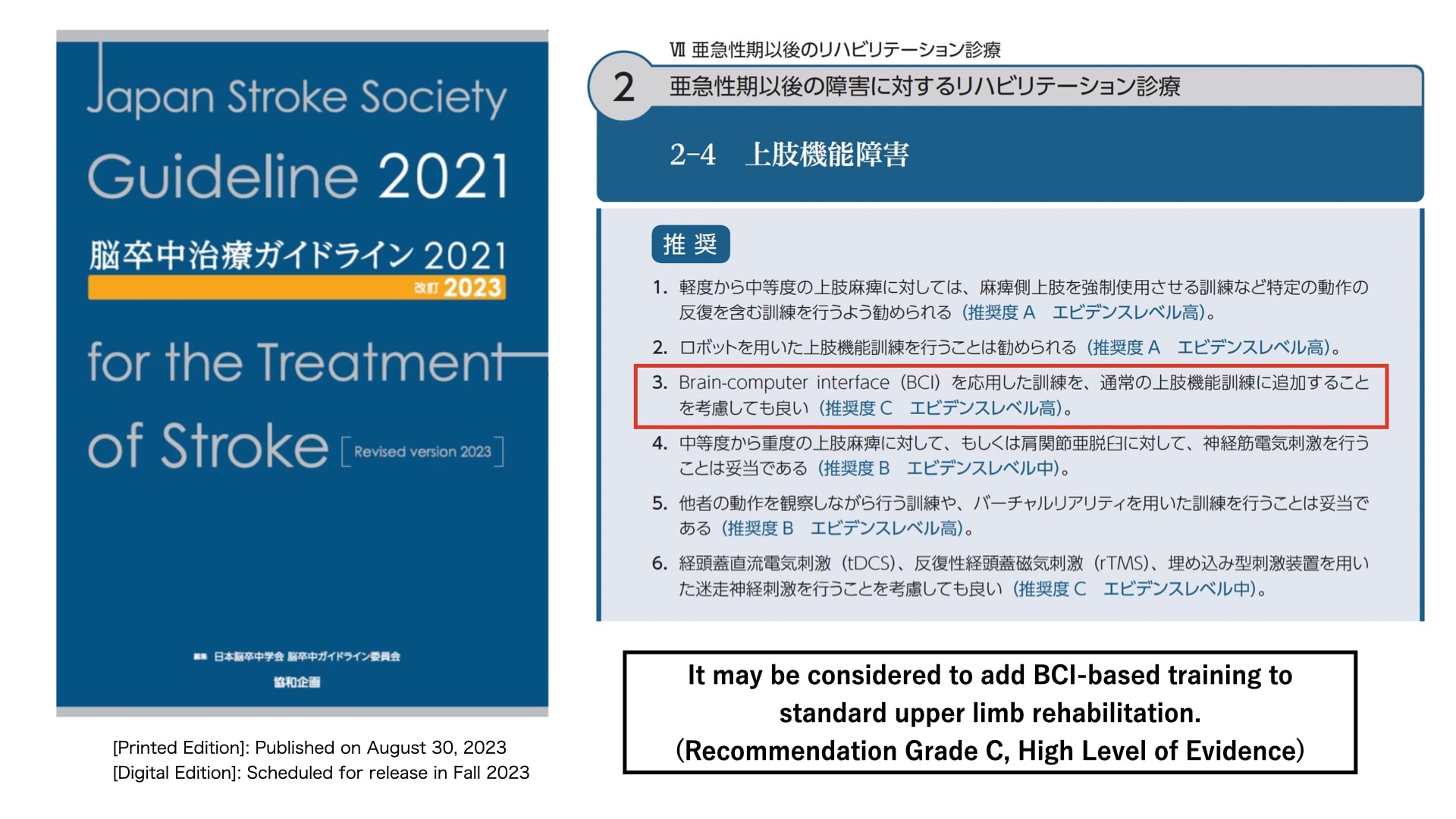
BCI training included in stroke treatment guidelines
Clinical Application | Stroke Treatment Guidelines (2021, Revised 2025)
- URL (Japanese):https://lifescapes.jp/
